Malawi’s Ministry of Health has confirmed three new cases of mpox in the capital city, bringing the national total to 11 since the country’s first reported case in April. Health officials say the outbreak is compounding already dire challenges in the nation’s fragile healthcare system, which has been rocked by recent cuts to U.S. government aid.
The Public Health Institute of Malawi stated the new patients, aged between 17 and 41, are currently under investigation to determine the source of infection and to trace contacts. The news comes as Malawi joins 15 other African nations battling mpox outbreaks amidst global vaccine shortages and strained medical infrastructure.
Health officials say the spread of the virus is being intensified by Malawi’s ongoing HIV crisis, which has worsened due to severe shortages of antiretroviral therapy (ART) caused by funding cuts. “A commonality about these cases is that some were immunocompromised,” said Richard Mvula, spokesperson for the Lilongwe district health office. Many patients have reportedly been forced to stop their HIV treatment due to depleted medication supplies.
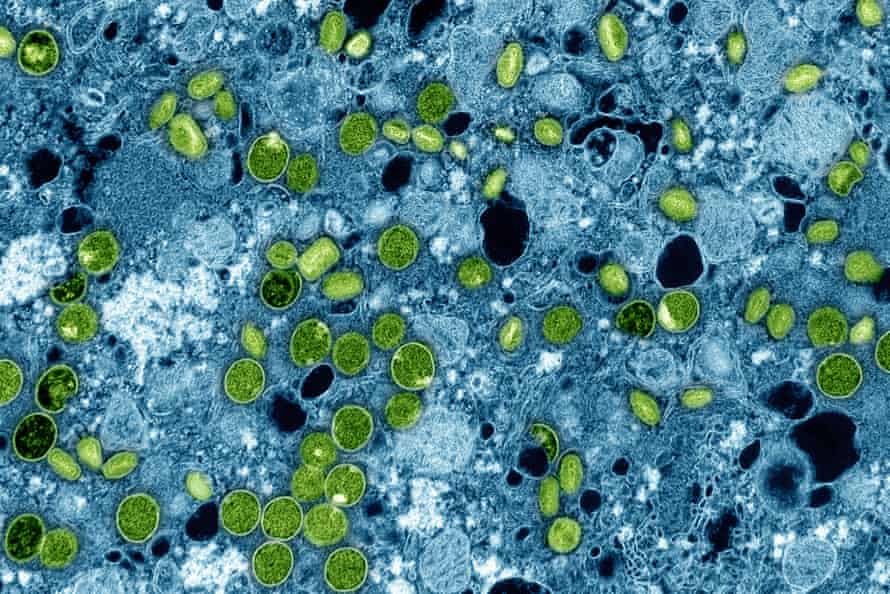
Mpox can cause more severe symptoms in people living with HIV, especially those with uncontrolled viral loads. Experts warn that the interruption of HIV treatment is fueling a dangerous overlap of health crises in one of the world’s poorest nations.
Malawi has been on high alert since mpox outbreaks first surged in parts of Africa in 2022. While most of the country’s cases have been confined to Lilongwe, a two year old child was recently diagnosed in Mangochi district, more than 240 kilometers from the capital.
The continent-wide situation remains alarming. According to the Africa Centers for Disease Control and Prevention (Africa CDC), more than 52,000 mpox cases and over 1,770 deaths have been recorded across Africa since January 2025. The organization estimates that 6.4 million vaccine doses are needed to curb the spread, yet only 1.3 million doses have been received so far.
Africa CDC officials also noted different viral clades circulating in different countries. While clade IIb is driving exponential case growth in Sierra Leone, clades Ia and Ib are dominant in the Democratic Republic of the Congo and surrounding nations.
Malawi’s health system has long struggled with underfunding, poor infrastructure, and shortages of trained staff and medical supplies. These challenges have worsened since the U.S. government slashed over $350 million in annual healthcare aid, affecting key programmes such as HIV prevention and treatment. In March, the Joint UN Programme on HIV and Aids warned that thousands of doses of HIV prevention medication were expiring unused, and that distribution of injectable PrEP had been limited to pregnant and lactating women only.
Knowledge about mpox among the general population remains low. In central Lilongwe, taxi driver Steven Banda admitted he only recently learned about the disease from a health official. “We don’t know much about it,” he said.
Medical professionals are calling for heightened awareness and preventive practices. Dr. Victor Mithi, president of the Society of Medical Doctors in Malawi, urged frontline workers to remain vigilant during clinical procedures. “It is a big concern,” he said, noting that the country’s communal culture, characterized by physical greetings and crowded housing, increases the risk of transmission.
Still, Mithi expressed cautious optimism. “With the lessons drawn from Covid-19 and other infectious diseases, we have the capacity to manage mpox at both clinical and community levels,” he said. “But the withdrawal of U.S. aid has left our healthcare system shaken. We did not build the internal capacity to sustain ourselves.”
As mpox continues to spread and vital funding remains uncertain, Malawi faces the uphill task of fighting a growing epidemic with limited tools and a system stretched to its breaking point.